By Farhan Malik, MD
Atlanta Innovative Medicine
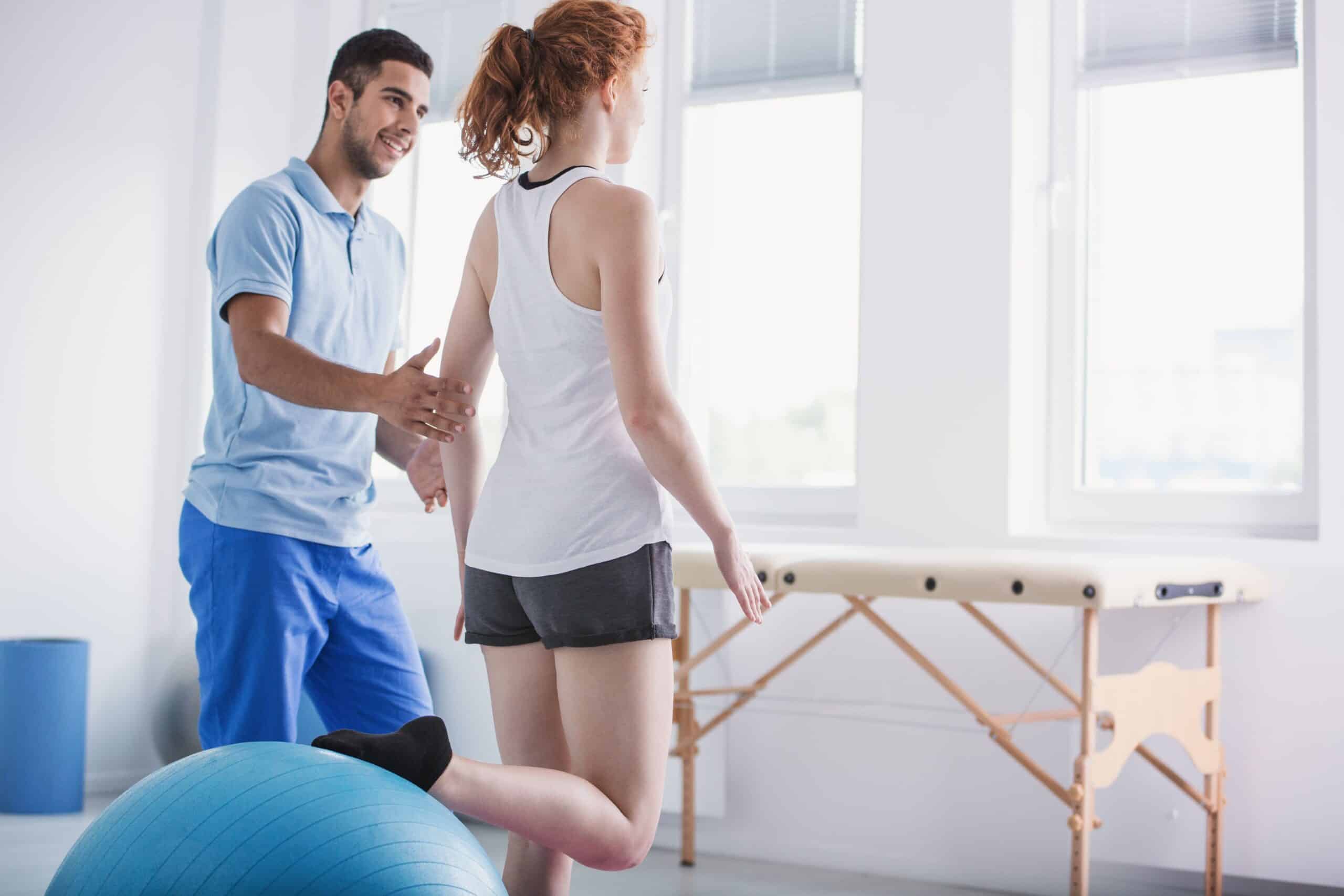
You’ve taken your first steps, learned to run, and logged countless miles in your lifetime, but after an injury, something as basic as walking can suddenly feel unfamiliar. That’s where gait training comes in: a focused, expert‑guided form of physical therapy that retrains how you walk and run by refining movement patterns, balance, and coordination. Think of it as a tune‑up for your stride—practical, precise, and unexpectedly empowering. For older adults, gait training does even more—it improves balance, reduces fall risk, and helps maintain independence and confidence in everyday activities, which directly supports overall health and quality of life.
If you’re thinking, “Walking is a basic skill—do I really need a professional to help me with it?”, consider this: small, expert-guided adjustments from a trained physical therapist can correct hidden flaws, speed recovery, and prevent the long-term wear and tear that trial-and-error practice can cause. Emerging evidence even shows that personalized gait training can provide pain relief comparable to medications and slow structural decline in conditions like knee osteoarthritis—outcomes you don’t typically get from solo practice.1
In this article, you’ll learn what gait training actually involves, how it might help you, which gait training exercises are commonly used in physical therapy, and what a typical training session looks like. Whether you’re recovering from injury, managing a chronic condition, or simply chasing a more confident, pain‑free walk, gait training can be a genuine game‑changer.
What Is Gait Training?
Gait training is a specialized form of physical therapy that focuses on improving how a person walks (and runs). The goal is to restore natural movement, alleviate pain, prevent re-injury, and enhance your quality of life. It’s more than just putting one foot in front of the other—gait training retrains your body to move efficiently, safely, and with good form by addressing posture and alignment, balance and stability, coordination, strength and endurance, and the speed and fluidity of movement. Exercises are tailored to your age, fitness level, and specific mobility challenges to restore a more natural, pain-free walking pattern.
Even without a recent injury, professional gait training can uncover small faults—foot strike, push‑off mechanics, or which muscles are doing the work—and teach a more efficient way to walk that protects your body instead of wearing it down. Older adults can benefit hugely from gait training, as better balance directly translates to greater independence.

Ready to walk without pain & strain? Schedule your complimentary 15-minute consultation with our physical therapy team today.
How Gait Training Improves Balance & Mobility
Imagine your body as a finely tuned machine: when one part isn’t working correctly, the whole system compensates, and other parts begin to strain. Gait training recalibrates that system to improve not only your walking but also your overall balance, mobility, and quality of life by:
- Strengthening key muscle groups: Exercises target the feet, legs, core, and upper-body muscles that support stable and efficient walking.
- Enhancing proprioception: Sharpens your body’s sense of position in space, thereby improving balance and reducing the risk of falls.
- Improving coordination: Repeated, specific practice helps the brain and muscles time movements more efficiently.
- Increasing confidence: Greater stability leads to increased confidence in daily activities, which in turn boosts mobility.
- Reducing pain: Better gait mechanics alleviate unnecessary stress on joints and muscles, often resulting in decreased hip and knee pain.
For older adults, these targeted corrections often translate into fewer falls, better mobility, and greater ability to stay active—factors strongly linked to improved physical and mental wellbeing.
Common Gait Training Exercises Used in Physical Therapy
The purpose of gait training is to get people walking better, safer, and more confidently. Physical therapists blend targeted strength, mobility, balance, and task-specific practice with sensory cueing and hands-on guidance to reteach efficient and reliable walking patterns. Working with a professional helps to reinforce correct movement, so practice transfers to everyday steps. Your physical therapy will likely include a mix of the following gait training exercises.
1. Walking practice (task-specific gait)
Directly targeting your timing, rhythm, and endurance, walking practice helps your skills transfer to daily life. Your therapist guides this process by providing timing cues, using metronomes or floor lines, and offering graded support—from harnesses and supports to less assistance—to help shape a safer, more efficient gait. Exercises such as treadmill walking, heel-to-toe (tandem) walking, and backward walking are used to help retrain your movement patterns.

2. Foot & ankle mobility and control
Restoring ankle mobility and proprioception is essential for safe and effective walking. Improving dorsiflexion and plantarflexion helps you clear the ground, achieve proper heel strike, and push off confidently. Your therapist will have you perform exercises such as ankle dorsiflexion and plantarflexion drills, assisted toe raises, and heel raises to foster strength and coordination in your ankles.
3. Lower‑limb strength
Building strength in your hips, thighs, glutes, and calves creates a supportive foundation for walking with confidence. It helps sustain stability, generate propulsion, and maintain consistent step length. Example exercises include step-ups, seated knee extensions, hip bridges, and side leg raises designed to enhance overall gait support. Your therapist will ensure you maintain proper form and load your muscles correctly during these exercises.
4. Balance, control, and weight-shifting
Improving control and proper weight transfer is crucial for safe and confident walking—especially on uneven surfaces and for preventing falls. Your therapist might have you practice balancing on one leg, shifting weight from one leg to the other, or using tools like wobble boards to challenge your balance. They will also use cues and guidance, such as visual markers, tactile support, and movement prompts, to help you establish the correct feel for even weight distribution and proper timing between the stance and swing phases of walking. Activities such as lateral stepping and marching in place help reinforce symmetry and coordination.

5. Core stability and trunk control
A strong, stable core supports efficient gait by stabilizing your pelvis and controlling your center of mass. Your therapist will guide you in building this strength with exercises like toe taps, knee-to-chest holds, and seated marching, all designed to reinforce the core strength that supports a natural walking pattern.
6. Functional & environmental practice
Simulating real-world challenges, such as stairs, curbs, and crowded sidewalks, helps build adaptability in everyday settings. Your therapist will use practice exercises that mimic real-life environments, such as stair negotiation, obstacle courses, side-stepping, and balance beam walking, to help prepare you to navigate these everyday challenges with confidence.

7. Neuromuscular facilitation & sensory cueing
Neuromuscular facilitation and sensory cueing involve using various types of signals—such as words, touches, sights, and sounds—to help your brain and body relearn how to walk smoothly and efficiently. Your therapist will combine these cues with activities like guided weight-shifting, walking to a beat, and walking along marked lines to improve your timing, coordination, and overall walking pattern.
8. Assistive device & orthotic training
When extra support is needed, your therapist will teach you how to use canes, walkers, or orthoses effectively. Proper handling, hand placement, and step strategies are emphasized, with hands-on guidance to build confidence and ensure safe, proper use. Examples include gait training with a cane or walker and walking with an ankle-foot orthosis (AFO), which helps you move confidently, safely, and independently.
Gait Training vs. Regular Walking: Why It Matters
If you can walk, why see a professional? Because gait training is more than just walking—it’s targeted, corrective, and progressive practice designed to build safe, efficient walking that transfers to real life. The key advantages of gait training with a physical therapist include:
- Focused Form Correction: A certified therapist is trained to detect and correct subtle movement faults (such as timing, foot placement, and hip position) that you’re unlikely to notice on your own.
- Personalized, Progressively Challenging Plans: When you work with a professional, your gait training program is tailored specifically to your needs, goals, and medical history. As you improve, your therapist can make exercises more challenging by increasing the load, complexity, speed, or environmental demands to ensure continuous progress in a manageable and engaging way.
- Safety and Fall Prevention: Physical therapists are trained to ensure safe progression, using support or assistive devices as needed, and taking precautions to reduce fall risk during practice. They will also instruct you on how to reduce falls at home, which has a direct impact on long-term health outcomes and quality of life for older adults.

The bottom line: regular walking builds fitness; gait training rebuilds walking itself, safely and with long‑term benefits.
When You Might Need Gait Training
If walking feels different, painful, or shaky, it’s a good time to consider professional gait training. Gait training helps a wide range of people regain safer, more efficient walking. It’s commonly recommended after stroke or other neurological events, following orthopedic surgery or injury, and for chronic conditions such as arthritis or multiple sclerosis. It’s also useful for anyone with balance problems or a history of falls, older adults with age-related mobility decline, individuals born with mobility-affecting conditions, and those learning to walk with prosthetics or orthoses. Even athletes benefit, as gait work can enhance performance and reduce the risk of injury.

At-Home Gait Training Tips & Maintenance
Professional guidance matters, but what you do between visits makes a big difference, too. Always stick to the home exercise program your therapist prescribes (this is absolutely essential, and they’ll remind you as often as you need!). Additionally, practice mindful walking during everyday activities: stand tall, cue a soft core, and notice heel‑to‑toe placement. Fold balance work into routines (stand on one foot while brushing your teeth, or walk heel‑to‑toe between rooms) and use simple tools like tape lines in a hallway to practice straight‑line walking.
Continue to strengthen the muscles that power gait with exercises such as squats, calf raises, and glute bridges. Ask your physical therapist for progressions and form cues to reinforce good mechanics and maintain proper posture. Stay active with short, regular walks or other aerobic activity to maintain endurance and mobility. As the weather cools, check out our tips for staying active and pain-free even in less-than-ideal weather conditions.

Finally, wear supportive shoes that fit well to protect your alignment and ensure comfort. Many specialty running stores, like Big Peach Running Co. and Road Runner Sports, right here in Atlanta, offer fit analyses to get you in the exact right shoe for you.

Subscribe for Expert Insights and Our Ebook
A Closer Look at Regenerative Medicine: Comparing Your Options Learn about treatment options like Platelet Rich Plasma (PRP), Prolozone Therapy, and Stem Cell Therapy.
When to Seek a Specialist for Gait Issues
If walking causes persistent pain, your stride looks or feels different than usual, you’re feeling unsteady, you’ve been diagnosed with a balance or coordination condition, or you’re struggling to regain normal walking after surgery or injury—it’s time to get specialist help.
If you’re unsure whether gait training is right for you, start with a complimentary consultation with our expert Atlanta Innovative Medicine team. We’ll listen to your goals, pinpoint what’s driving the problem, and guide you through next steps.
Take the first step—book a consultation with our team today. Call 770.416.9995 or click to schedule. Let us help you walk better, safer, and more confidently.
Sources:
1 Lerner, E., University of Utah (2025, August 24). No Pills, No Surgery: Scientists Discover Simple Way To Relieve Arthritis Pain. SciTechDaily. https://scitechdaily.com/no-pills-no-surgery-scientists-discover-simple-way-to-relieve-arthritis-pain/
Quizzes
Are you a candidate for Regenerative Medicine?
Regenerative medicine can be an effective therapy and treatment option for lasting pain relief for a variety of conditions like osteoarthritis of the knee, hip or shoulder; ACL or meniscus tears; tennis or golfer’s elbow; chronic neck and back pain; and more.
Is it right for you and your condition? Take 1 minute to answer a few “yes or no” questions that help to assess if you might be a candidate for PRP, stem cell or other nonsurgical regenerative treatments.
Are You a Stem Cell Candidate for Your Joint or Spine Damage?
Are you a candidate for Platelet Rich Plasma (PRP) Therapy?
Do I have nonsurgical options for my injured or aging joints?
Take the Pain Medications Risk Quiz
Regenerative Medicine.
Reimagined
- Advanced hybrid therapies, including Mesenchymal Stem Cell therapy combined with different mechanisms of action that synergistically come together to support ultimate healing
- More powerful PRP that’s customized, amplified and personalized
- Therapies delivered by an experienced, compassionate team comprised of multidisciplinary experts in traditional and alternative medicine working as your team: Medical Doctors, Nurse Practitioners, Physiotherapists and Chiropractors
- Advanced training through the American Academy of Orthopedic Medicine, the American Osteopathic Association of Prolotherapy Regenerative Medicine, and more
All content of this page is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider. Individual results may vary. Your medical professional can explain all the risks and potential benefits of any therapy based on your specific circumstances. At this time regenerative therapies are not FDA approved. Neither Atlanta Innovative Medicine nor its physician affiliates promise regenerative therapies as a cure for any condition, disease, or injury.
Other Atlanta Areas We Service:
© 2024 Atlanta Innovative Medicine, LLC. All Rights Reserved. AIM Scholarship Opportunity